From the age of 50, some stem cells take control of the blood, causing it to lose diversity, and we are more prone to illness.

In the long race toward aging, some stem cell clones in our bodies take control of blood production, while others disappear or remain residual. Competition between stem cells means that, as we age, our blood system changes and deteriorates, loses diversity, and makes us more vulnerable to disease.
A new Spanish study published today in the journal 'Nature', led by researchers from the Institute for Research in Biomedicine (IRB Barcelona) and the Centre for Genomic Regulation (CRG), explains how, in both humans and mice, age shapes our blood system, how a few stem cells outcompete their neighbors in this process and take control of blood production, resulting in a reduction in stem cell diversity and a predominance of those linked to chronic inflammation.
"The loss of diversity that occurs with age is correlated with negative consequences," explains researcher Lars Velten , group leader at the CRG in Barcelona who co-led the study. The major contribution of the research, which, according to the authors, "will change the textbooks," is that these changes in the blood are detectable from age 50 and become "universal" from age 60, meaning they are experienced by everyone.
The discovery opens the door to the design of new strategies to detect early signs of unhealthy aging long before symptoms appear, thus helping to prevent diseases linked to aging and blood, such as myeloid leukemia, cardiovascular disease, and immune disorders . It also paves the way for the design of potential therapies to delay aging in humans, an area that has traditionally focused on animal models.
“Our blood stem cells compete for survival. In youth, this competition creates a rich and diverse ecosystem , but in old age, some cells disappear entirely. A few stem cells take over and work twice as hard to compensate, reducing diversity and weakening the blood system’s resilience. Diverse stem cells can respond to different stresses, so the dominance of a handful of clones makes the entire system more fragile. The more diverse a system is, the easier it is to respond to change,” Velten explains.
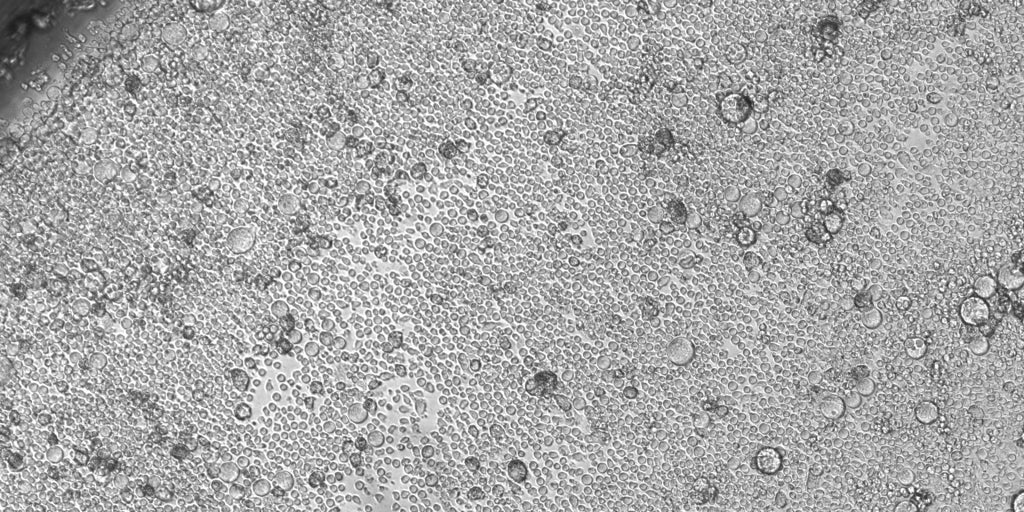
In young people, there are between 50,000 and 200,000 active blood stem cells that produce 100 to 200 billion new cells every day. Tracing each of these back to its original stem cell has so far only been possible in animal models, requiring genetic modification of the DNA, "something unfeasible and unethical in humans," according to the authors of the study.
So the team turned to epimutations : changes in chemical marks (methylations) that attach to DNA and tell the cell which genes to activate or silence. When a parent cell divides, these marks are copied to the daughter cells, leaving a permanent "barcode" that researchers can read to reconstruct the cell's family tree.
"Our cells carry genetic changes that collectively make us unique individuals. But within each individual, we also carry a mosaic of genetic and epigenetic alterations. These alterations are inherited within each family of cells, which, although they end up performing different functions, share the signatures that link them to a common ancestral stem cell. We have finally been able to construct the epigenetic family tree by reading the information written directly in the DNA of each cell," comments Alejo Rodríguez-Fraticelli, ICREA researcher at IRB Barcelona and co-author of the study.
"This new tool allows us to know the cell's surname, what type of cell it is, whether it has expanded, and what it's doing," the researcher notes. "If we understand why some cell lines expand and others don't, we may be able to prevent these expansions in the future, or make the expansion of some clones more uniform, which could improve healthy life spans," Rodríguez-Fraticelli explains.
To address this challenge, researchers have developed a technique called 'EPI-Clone' , which reads these methylation barcodes in each cell. "DNA methylation works like a binary code: every site in the genome is either methylated or not, like a 1 or a 0," explains Michael Scherer, a bioinformatician and co-first author of the work at the CRG, now a group leader at the German Cancer Research Center (DKFZ). "This simple on-off information can be transformed into a natural barcode, one that each stem cell passes on to its descendants. Five years ago, I wouldn't have believed this possible at single-cell resolution, across tens of thousands of cells. It's been a huge leap forward in technology," he adds.
In young blood, thousands of different stem cells contribute to a rich and diverse set of red blood cells, white blood cells, and platelets. However, EPI-Clone revealed that in aged mice, up to 70% of blood stem cells belonged to just a few dozen large clones . The situation is similar in humans. The study revealed that, starting at age 50, many blood stem cells begin to disappear, and larger clones begin to take over. Starting at age 60, the change becomes even more pronounced.
"The shift from diversity to the dominance of a few isn't random; it moves like clockwork," notes Dr. Indranil Singh , co-first author and researcher at IRB Barcelona, now at the Broad Institute of Harvard and MIT. "By age 50, you can already see it starting, and after age 60, it seems almost inevitable."
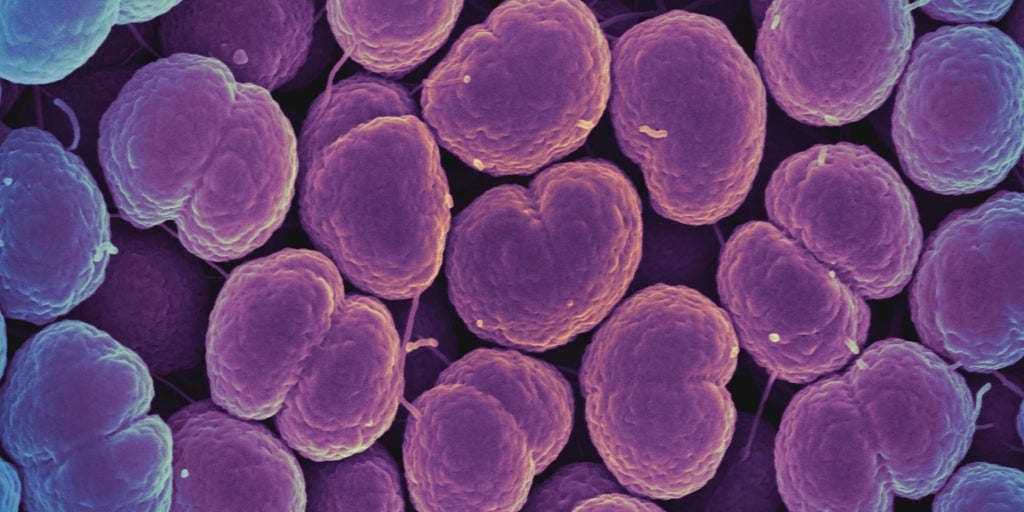
The study also found that some large clones harbored mutations related to clonal hematopoiesis , a process in which some blood stem cells acquire mutations that allow them to grow and multiply faster than others. This phenomenon becomes more common with age and has been shown to increase the risk of heart disease, stroke, and leukemia . However, many of the dominant clones identified by EPI-Clone did not have any known mutations, suggesting that clonal expansion is a general feature of blood aging, not just a sign of cancer risk. "Previous research has focused on mutations localized to cancer genes, known as 'pre-cancer,'" the authors emphasize. "In contrast, our work suggests that this process is universal, at least in the blood."
"This means," they add, "that in the future, doctors could one day assess clonal behavior itself for early detection, offering them a way to monitor how a person's blood stem cell pool is aging years before any disease develops. People with a more rapid loss of diversity or a rapid expansion of at-risk clones could be targeted for preventive care."
The study also revealed that, in both aged humans and mice, many of the dominant clones show a preference for producing myeloid cells . These are immune cells linked to chronic inflammation. Previous studies in mice have shown that selectively removing myeloid-biased stem cells can increase the production of infection-fighting lymphocytes and improve immune responses.
However, to study anti-aging therapies in humans, researchers would first have to identify which clones are problematic, something they admit "has not been possible so far" and is not possible with their technique.
"We've only demonstrated what's possible," concludes Rodriguez-Fraticelli . "Now the goal is to perfect EPI-Clone so it can boost clinical research efforts." In this sense, one of the current challenges is to reduce the cost of the technique so it can be used in population screening and protect the population from diseases linked to aging. "Currently, the cost is around €5,000 per patient," the researchers point out, who believe it's feasible that within ten years everything they've discovered will reach the clinic.
The study has received funding from the Spanish Association Against Cancer , CRIS against cancer, the European Research Council (ERC), the European Hematology Association , the La Caixa Foundation , the Spanish Ministry of Science and Technology , and the Generalitat of Catalonia .
abc